Labeling exercise 8 1 patient id and blood specimen label – In the realm of healthcare, precision and accuracy reign supreme. Labeling exercise 8.1 places the spotlight on patient identification and blood specimen labeling, highlighting their pivotal role in ensuring patient safety and reliable diagnostic outcomes. Join us as we delve into the intricacies of this critical process, exploring its significance, best practices, and legal implications.
Proper labeling forms the cornerstone of effective patient care. It safeguards patient identity, facilitates accurate specimen identification, and ensures seamless communication among healthcare professionals. By adhering to established protocols, we minimize errors and promote optimal patient outcomes.
Patient Identification Label: Labeling Exercise 8 1 Patient Id And Blood Specimen Label

Patient identification labels are used to uniquely identify patients and their medical records. They are typically placed on the patient’s wrist or ankle and contain information such as the patient’s name, date of birth, and medical record number.
The accuracy and completeness of patient identification labels are essential for patient safety. Incorrect or incomplete labels can lead to medical errors, such as misidentification of patients or incorrect administration of medications.
Blood Specimen Label
Blood specimen labels are used to identify blood samples and the patient from whom they were collected. They typically contain information such as the patient’s name, date of birth, medical record number, and the date and time the sample was collected.
The accuracy and completeness of blood specimen labels are also essential for patient safety. Incorrect or incomplete labels can lead to misidentification of samples or incorrect test results.
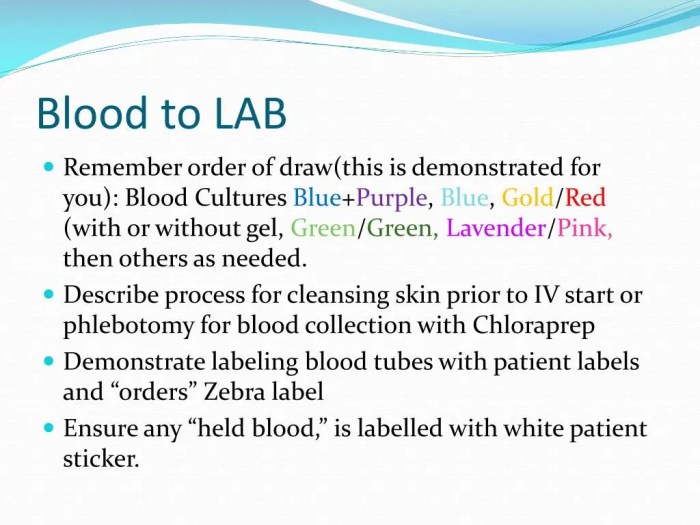
Labeling Procedure
The labeling procedure should be followed carefully to ensure the accuracy and completeness of the labels.
- The patient’s name and date of birth should be verified against the patient’s identification band or other reliable source.
- The medical record number should be accurately transcribed from the patient’s chart.
- The date and time the sample was collected should be accurately recorded.
- The labels should be securely attached to the patient or the blood specimen.
Common errors that can occur during the labeling procedure include:
- Transcription errors
- Omission of information
- Incorrect placement of the labels
Quality Control, Labeling exercise 8 1 patient id and blood specimen label
Quality control measures should be in place to ensure the accuracy and completeness of the labels.
- Regular audits and inspections should be conducted to verify the accuracy of the labels.
- Staff should be trained on the proper labeling procedure.
- Technology, such as barcode scanners, can be used to improve the accuracy of the labeling process.
Potential risks associated with labeling errors include:
- Misidentification of patients
- Incorrect administration of medications
- Misidentification of blood samples
- Incorrect test results
Best Practices
Best practices for labeling patient identification and blood specimen labels include:
- Use high-quality labels that are resistant to smudging and fading.
- Use a large, easy-to-read font.
- Include all of the necessary information on the label.
- Use technology, such as barcode scanners, to improve the accuracy of the labeling process.
- Train staff on the proper labeling procedure.
Legal and Regulatory Considerations
There are legal and regulatory requirements for labeling patient identification and blood specimen labels.
- The Joint Commission requires that patient identification labels be used on all patients.
- The Centers for Medicare & Medicaid Services (CMS) requires that blood specimen labels contain certain information, such as the patient’s name, date of birth, and medical record number.
- Non-compliance with labeling requirements can result in fines or other penalties.
Examples of successful legal challenges related to labeling errors include:
- In 2015, a patient was awarded $1 million after a hospital misidentified her blood sample and gave her the wrong transfusion.
- In 2017, a hospital was fined $100,000 after a patient died due to a mislabeled blood transfusion.
FAQ Insights
Why is accurate labeling so crucial in healthcare?
Accurate labeling ensures correct patient identification, eliminates specimen mix-ups, and supports effective communication among healthcare providers, reducing the risk of errors and improving patient safety.
What are the key components of a patient identification label?
Typically, a patient identification label includes the patient’s full name, date of birth, medical record number, and other relevant identifiers.
How can technology enhance the labeling process?
Electronic health records (EHRs) and barcode systems can streamline labeling, reduce errors, and improve the efficiency of patient identification and specimen management.